Depression is far more than just a series of bad days or moments of sadness. It is a complex and pervasive mental health condition that affects not only a person’s mood and emotional state but also the very structure and function of the brain. As someone who has battled with depression firsthand, I’ve often wondered how it could influence my thoughts, actions, and even my ability to experience joy or motivation. During my own struggle with depression, I found myself in a constant state of emotional numbness and mental fog. Simple tasks felt overwhelming, and it was as though my mind was locked in a loop of negativity, unable to break free. This led me to dive deeper into the science behind depression and its profound effects on the brain.
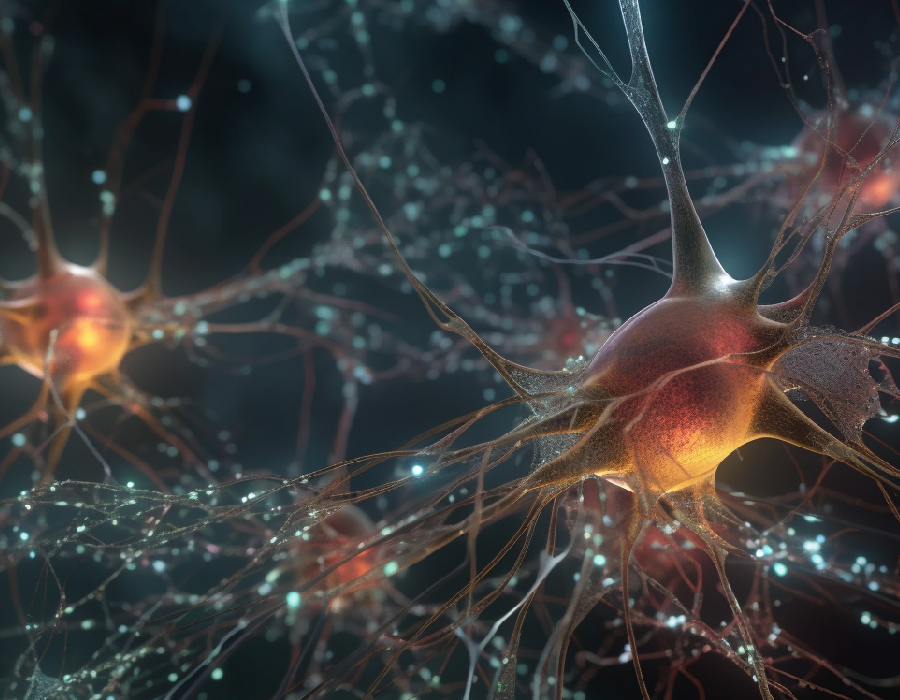
Through my research, I discovered that depression induces significant changes in key areas of the brain, particularly those involved in regulating emotions, memory, and cognitive function. The experience of depression isn’t just about emotional distress; it’s about how it physically alters the brain. These changes can lead to cognitive impairments, emotional regulation issues, and difficulty forming new memories or processing information. While it can feel like there is no way out of the darkness, science reveals that the brain has a remarkable ability to adapt and heal itself over time. This phenomenon, known as neuroplasticity, offers hope to those living with depression.
As we dig into the relationship between depression and brain structure, it becomes clear that understanding these changes is critical for developing more effective treatments. In this article, we will explore the specific areas of the brain most affected by depression, including the prefrontal cortex, hippocampus, and amygdala. By examining how depression impacts neuroplasticity—the brain’s ability to reorganize itself—we can better understand why depression affects people in such a deep and lasting way. Ultimately, we will also discuss the ways in which neuroplasticity can be supported and restored, offering new hope for healing.
READ: How Psychedelics (Shrooms) Helped Me Overcome Depression and PTSD

In-Depth Explanation
Depression, clinically known as major depressive disorder (MDD), is a multifaceted mental health condition characterized by persistent sadness, loss of interest, and a range of cognitive and physical symptoms. It goes beyond emotional and mental suffering, influencing the very brain structures responsible for cognition, emotion, and behavior. Emerging research has illuminated several key brain regions that are affected by depression, including the prefrontal cortex, hippocampus, and amygdala. These brain areas play a vital role in how we think, feel, and interact with the world. So, let’s take a closer look at how depression impacts each of these regions, and how these changes contribute to the overall experience of the disorder.
Prefrontal Cortex: The Decision-Making Center
The prefrontal cortex is one of the most critical areas of the brain, responsible for executive functions such as decision-making, attention, and regulating social behavior. It’s the part of the brain that helps us plan, solve problems, and control our emotions in social interactions. When depression sets in, however, studies show that this region experiences hypoactivity, meaning it’s not functioning at full capacity. This reduction in activity can manifest as difficulties in emotional regulation, trouble making decisions, and challenges in focusing on tasks. For someone dealing with depression, simple decisions can feel overwhelming, and the inability to control emotions can lead to feelings of helplessness. This disruption in the prefrontal cortex is a significant factor in why depression can impair daily functioning and overall quality of life.
READ: Healing Depression Without Medication: A Holistic Approach

Hippocampus: The Memory and Learning Hub
The hippocampus, often described as the brain’s memory center, is essential for forming new memories and navigating our environment. In depression, however, this region can undergo structural changes that impact its functionality. One of the most notable effects of depression on the hippocampus is its atrophy, or shrinkage. Chronic exposure to stress hormones like cortisol, which are often elevated in those suffering from depression, can lead to this reduction in hippocampal volume. As a result, individuals with depression often experience memory impairments, struggling with recalling past experiences or forming new memories. This atrophy is more than just a structural change; it also contributes to cognitive challenges such as difficulty concentrating or learning new information. The hippocampus’s decreased ability to function properly in depressed individuals might explain why many find themselves trapped in a cycle of negative thoughts and memories, unable to break free from the fog of depression.
Amygdala: The Emotional Center
The amygdala plays a central role in processing emotions such as fear, pleasure, and anger. It’s particularly involved in the brain’s response to stress and emotional stimuli. In people with depression, the amygdala tends to be hyperactive. This means it’s overly sensitive to negative stimuli, which can result in heightened feelings of sadness, anxiety, and fear. Essentially, the amygdala is on overdrive, amplifying emotional responses to situations that might otherwise seem manageable. This hyperactivity is believed to contribute to the persistent feelings of anxiety and sadness that are hallmarks of depression.
As someone who has lived with low-grade, persistent depression for years, I became curious about the relationship between magic mushroom and dysthymia—a chronic form of depression that often goes overlooked. I learned that psilocybin’s effects on the amygdala could help reduce this overactivation, potentially breaking the cycle of emotional stagnation that characterizes dysthymia. For individuals experiencing depression, the amygdala’s heightened sensitivity often leads to a feeling of being stuck in an emotional state, where negativity dominates every aspect of life, from relationships to self-esteem. Emerging research and personal anecdotes alike suggest that psychedelics like magic mushrooms may offer new hope for those of us battling this quieter, more enduring form of depression.
Check out this magic mushroom!!
A.P.E Psilocybin Chocolate Bar
$60.00Dried Penis Envy Magic Mushrooms
$60.00 – $240.00Price range: $60.00 through $240.00Golden Teacher Gummies for Microdosing
$25.00
Neuroplasticity and Depression: Can the Brain Heal?
Neuroplasticity, often referred to as the brain’s ability to rewire itself, plays a crucial role in how we experience and overcome depression. At its core, neuroplasticity allows the brain to adapt to new experiences, form new connections, and even compensate for damaged areas of the brain. However, depression can significantly impair this natural ability, leading to lasting changes in brain structure and function. Understanding how neuroplasticity interacts with depression offers a glimpse of hope for those seeking recovery.
The Impact of Depression on Neuroplasticity
Depression is not simply an emotional condition; it is a neurobiological one that affects the very architecture of the brain. Chronic depression can lead to disruptions in neuroplasticity, manifesting as diminished synaptic connections, neuronal atrophy, and impaired neurogenesis. These disruptions prevent the brain from adapting to new, healthier patterns of thinking, feeling, and behaving, which is why depression often becomes a vicious cycle that is difficult to break. Essentially, depression can freeze the brain in a negative, maladaptive state, making it harder to experience joy, motivation, and cognitive clarity.
Research has shown that prolonged exposure to high levels of stress hormones, like cortisol, can severely impact neuroplasticity. Elevated cortisol levels, often seen in individuals with chronic depression, inhibit the formation of new neural connections and lead to the shrinking of neurons, particularly in key brain areas like the hippocampus and prefrontal cortex. This impairs memory, decision-making, and emotional regulation, making it more challenging for those suffering from depression to engage in positive experiences or effectively manage their emotions.
READ: Are Magic Mushrooms Good For Anxiety And Depression: An In-Depth Look
Synaptic Dysfunction: The Breakdown of Communication
Synapses are the communication points between neurons, and their proper functioning is essential for everything from basic motor control to complex cognitive processes like memory and emotional regulation. In depression, synaptic dysfunction is common, and the reduction in synaptic formation is one of the most significant barriers to recovery. The brain’s inability to form new, healthy connections can leave individuals with depression feeling mentally “stuck,” as if their thoughts and emotions are endlessly repeating in the same negative loops.
When synaptic activity is reduced, it also leads to poorer communication between different regions of the brain. This breakdown in connectivity is particularly detrimental in areas responsible for mood regulation, like the prefrontal cortex and amygdala. The prefrontal cortex, which is vital for executive functions like decision-making and emotional control, relies heavily on strong synaptic connections to manage and regulate emotions. When synapses are weakened or lost, individuals may find it harder to control emotional responses or make decisions, further exacerbating the feelings of helplessness and despair associated with depression.
Neuronal Atrophy: Shrinkage of Critical Brain Regions
Another key feature of depression is neuronal atrophy, or the shrinking of brain cells, which often occurs in regions that are vital for cognitive and emotional health. Two major brain areas that are especially impacted by depression are the hippocampus and prefrontal cortex. The hippocampus, essential for memory formation and emotional regulation, has been found to shrink in individuals with chronic depression. This reduction in size is believed to be a result of prolonged exposure to stress hormones, particularly cortisol, which can damage and shrink neurons over time.
Similarly, the prefrontal cortex, which helps manage executive functions such as decision-making, impulse control, and emotional regulation, can also experience atrophy during prolonged periods of depression. As this region becomes less effective, individuals may experience difficulty focusing, making decisions, or managing their emotions, all of which are common symptoms of depression. The shrinkage of these critical brain regions can create a feedback loop, where the individual’s impaired cognitive and emotional functioning further perpetuates the depressive state.
READ: Psilocybin Mushrooms as a Potential Treatment for Depression: Current Research and Insights

Decreased Neurogenesis: The Decline in New Neurons
Neurogenesis is the process by which new neurons are generated, particularly in the hippocampus. This process is crucial for learning, memory, and overall brain health. In healthy individuals, neurogenesis allows the brain to adapt to new experiences, form new memories, and maintain cognitive flexibility. However, depression has been shown to reduce the production of new neurons in the hippocampus, a key brain region responsible for forming new memories and managing emotions.
Lowered neurogenesis in individuals with depression means that the brain is less able to create new pathways for positive emotional experiences or adaptive coping mechanisms. This stagnation in the brain’s ability to regenerate itself can contribute to feelings of hopelessness, as individuals may struggle to envision or experience improvement. In addition, impaired neurogenesis limits the brain’s capacity to recover from the structural and functional damage caused by depression, making it harder for individuals to experience long-term relief from their symptoms.
Can Neuroplasticity Be Restored?
While depression can cause significant impairments in neuroplasticity, the brain is not a static organ. New research suggests that neuroplasticity can be restored, even in the midst of depression, with the right interventions. Treatments such as therapy, medication, exercise, and mindfulness practices have been shown to support and enhance neuroplasticity, promoting the formation of new neural connections and the regeneration of brain regions affected by depression.
One of the most promising interventions for restoring neuroplasticity is the use of psychedelics, particularly psilocybin, which has been shown to enhance neuroplasticity and promote the growth of new neurons. Studies have found that psilocybin can stimulate brain regions involved in emotional regulation and cognition, helping individuals with depression break free from negative thought patterns and emotional states. This suggests that psychedelics may offer a novel treatment approach for those whose depression has caused significant neurobiological damage.
A New Hope for Healing
While depression may significantly impair neuroplasticity, the brain’s ability to heal itself should not be underestimated. With the right treatment and support, it’s possible to restore brain function and create new, healthier neural connections. Psychedelics, alongside other therapies and lifestyle changes, offer a promising path toward healing and recovery. For those who have struggled with the cognitive fog and emotional numbness of depression, there is hope for a brighter, more balanced future.
READ: Psilocybin and Seasonal Affective Disorder: Can Magic Mushrooms Light Up the Winter Blues?
Take Control of Your Mental Health with Magic Mush: A Pathway to Healing
In this article, we’ve explored how depression impacts brain structure and function, focusing on regions like the prefrontal cortex, hippocampus, and amygdala. Depression’s effects on brain activity, such as hypoactivity in the prefrontal cortex and hyperactivity in the amygdala, explain the cognitive and emotional struggles that many individuals face. These alterations in brain structure and connectivity, including hippocampal atrophy, are crucial to understanding why depression isn’t just an emotional experience but also a physiological one. Neuroplasticity offers hope, as the brain’s ability to reorganize itself can potentially restore balance and mitigate the negative impacts of depression.
At Magic Mush, we believe in the power of psychedelics, particularly magic mushrooms, to support mental health and promote healing. With the research-backed potential of psilocybin to enhance neuroplasticity, the therapeutic use of dried magic mushrooms is becoming an increasingly popular choice for individuals seeking relief from depression and other mental health challenges. Our high-quality products, rigorous testing, and commitment to safe usage can provide you with the tools to begin your journey toward emotional and cognitive restoration. Whether you are looking to explore the benefits of psychedelics or seeking guidance on how to use them responsibly, Magic Mush is here to guide you every step of the way.
Magic Mush is dedicated to not only providing top-tier products but also creating an environment where education and community thrive. By challenging the stigma surrounding magic mushrooms, we empower individuals to safely explore their therapeutic potential. We’re more than just a product provider; we’re a partner in your mental health journey. Our seamless delivery in Toronto and Ottawa experience ensures privacy, and our exceptional customer support team is always available to assist you. Discover the transformative power of psychedelics with Magic Mush and begin your path to healing today.


